作者简介:倪伟勇(1982—),男,主检法医师,大学本科,研究方向为法医病理学和法医临床学。 E-mail:30083507@163.com
目的 对肋骨骨折的法医临床鉴定时间进行探讨。方法 对40例定期复查的肋骨骨折鉴定案件的CT表现和时间相关性进行研究。结果 26例被鉴定人外伤后2、4、6w CT检查所见的肋骨骨折部位数量有增多趋势,外伤4w后检查所示骨折部位数量趋于稳定。复查发现的肋骨骨折有79.3%表现为肋骨内侧或者外侧局部轻微的骨皮质断裂不完全性骨折,20.7%未能观察到骨折线,仅表现为局部密度增高和骨痂生长。结论 对肋骨骨折鉴定案例,在外伤4w后复查CT再进行人体损伤程度鉴定,可以有效避免损伤认定发生遗漏或鉴定意见出现错误。
Objective Rib fracture is a common injury in clinical forensic identification. According to the current injury degree and disability grade identification standard, different counts of rib fracture will result in different identification of injury degree and disability grade. The theoretic exploration of identification time of rib fracture can give an appropriate identification time for forensic clinical identification staff and avoid missed diagnosis or mistakes.Methods A retrospective study of 40 injury cases involved in rib fracture from 2011 to 2013 in Lishui was conducted. Chest multi-slice CT scanning was performed right immediately, and 2, 4, 6 weeks after injury, respectively. The correlation between the CT findings and timing was studied. The count and location of rib fracture were calculated for each CT examination. The missed diagnosis cases were classified. Bone fractures associated with both fracture line and callus growth and bone fracture with callus growth only in CT scanning were differentiated. The reason for the change of rib fracture count was analyzed.Results Of the 40 cases, 14 and 26 cases showed no changes and an increase in rib fracture sites, respectively. In the newly found 87 rib fractures by reexamination, 62% of them (54) were anterior to the anterior axillary line, 25%(22) were between the anterior axillary line and the posterior axillary line, 17%(11) were posterior to the posterior axillary line. Fracture lines and callus growth could be seen in 69 of the 87 rib fractures. All of them were incomplete fractures, which manifested as mild local interrupted bone cortex in the internal or external sites of ribs. Only local callus growth without obvious fracture lines could be seen in the other 18 fracture sites, which all located on the 2~7 anterior ribs. The count of rib fracture increased in 26 patients with CT scanning in 2 and 4 weeks following injury, while it tended to be steady after 4 weeks.Conclusions Fracture healing can be divided into three stages, including organization of hematoma stage, porotic stage and callus remodeling stage. In the early stage of rib fracture, the fracture line becomes more obvious by the breathing movement, organization of hematoma and the process of osteoclast eliminating the dead bone. But rib fracture may be missed diagnosis because of the unobvious fracture line in the early stage after injury. Rarefaction of bone and thin of bone cortex are main factors which is caused by the old age or the position of anterior rib to make the fracture line unobvious to display in CT images. As the repairing of fracture and calcium deposition in the callus, a gradual increase in density can be found in CT scanning. The direction of the fracture line close to the axle of the CT scanning could cause missed diagnosis of the hairlike fracture line. The thickness of layer over 1mm of CPR and MPR images would easily cause missed diagnosis. Our study shows that injury degree identification followed by CT examination in 4 weeks after injury in individuals with rib fractures is recommended because rib fracture site could be confirmed by callus growth. Missed diagnosis or mistakes can effectively be avoided in this way.
肋骨骨折是法医临床鉴定中较常见的损伤之一, 《人体损伤程度鉴定标准》颁布施行之后, 肋骨骨折部位由于数量上的差别存在轻伤一级、轻伤二级和轻微伤三个损伤程度结果; 《道路交通事故受伤人员伤残评定》(GB18667-2002)中, 由于肋骨骨折数量的差别存在Ⅷ 级、Ⅸ 级、Ⅹ 级三个伤残等级; 《人体损伤残疾程度鉴定标准(试行)》2.9.26也规定了5根以上肋骨骨折构成九级残疾。
本文通过对40例定期复查的肋骨骨折鉴定案例多层螺旋CT检查所发现的骨折部位与时间的关系进行回顾研究, 对肋骨骨折的鉴定时间进行探讨, 为法医临床鉴定人员选择适宜的鉴定时间, 避免认定的损伤出现遗漏或鉴定意见出现错误提供了参考。
对丽水市2011年~2013年受理的肋骨骨折案件中定期复查的40例案例进行回顾, 上述被鉴定人均在外伤后2、4、6w复查胸部CT。其中女性9例, 年龄45 ~62岁, 平均年龄48.4岁; 男性31例, 年龄26~78岁, 平均年龄49.7岁。
以观察到骨折线或者骨痂生长为判定骨折的标准。对上述被鉴定人外伤后当日及外伤后2、4、6w的胸部CT片进行复阅, 复查扫描仪器为GE Brightspeed Elite 16层螺旋CT或Philips Brilliance 16层螺旋CT。
定期复查的40例中, 有14例经复查所见肋骨骨折部位无变化, 占35%; 有26例经复查所见肋骨骨折部位有增多, 占65%。复查所见肋骨数量及变化情况见表1。
| 表1 复查所见肋骨数量及变化情况 Table 1 Changes of rib fracture quantity by reexamination |
经复查新发现的肋骨骨折位于腋前线之前的54处, 占62%; 腋后线至腋前线22处, 占25%; 腋后线之后11处, 占17%。复查所见肋骨骨折部位、数量及变化情况见表2。
| 表2 复查所见肋骨骨折部位、数量及变化情况 Table 2 Changes of rib fracture position and quantity by reexamination |
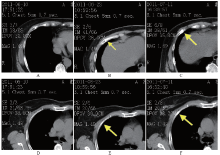
经复查新发现的87处肋骨骨折, 其中69处可观察到骨折线和骨痂生长, 均为不完全性骨折, 表现为肋骨内侧或者外侧局部轻微的骨皮质断裂(见图1A、B、C), 占79.3%; 18处仅观察到局部的骨痂生长(见图1D、E、F), 未见明显骨折线且均位于2~7肋骨前肋, 占20.7%。
肋骨为细长弓状的扁骨, 共12对, 呈系列斜行骨弓排列, 在前面通过肋软骨与胸骨衔接, 后面与胸椎构成胸肋关节。第1~7肋与胸骨直接相连称真肋; 第8~12肋不与胸骨直接相连称假肋; 其中第11、12肋因末端游离又称浮肋。肋骨之间借助相互交错的肋间肌和肋间外肌相互作用近似于弯曲平行排列, 当肋骨受力后超过肋骨的弹性强度极限便发生骨折, 肋骨的骨折多系弯曲变形所致。
肋骨骨折在胸部外伤中最为常见。肋骨骨折的愈合可以分为三个阶段:血肿机化期、骨痂形成期和骨痂塑形期[1]。肋骨骨折后, 早期由于呼吸运动以及局部血肿机化、破骨细胞清除死骨, 部分细微的骨折线变得明显; 血肿机化后, 骨折端部位骨膜反应为膜成骨痂, 血肿机化形成的纤维血管性肉芽组织大部分变为软骨骨痂, 随着骨痂中钙盐逐步沉积, 在CT影像所见上密度逐渐增高, 容易被识别。
随着多层螺旋CT的普及, 以及容积再现(VR)、曲面重建(CPR)、表面遮盖法(SSD)等重组技术的广泛应用, 肋骨骨折的早期检出率有了很大的提高。当肋骨骨折线比较明显时常规X线平片即可发现; 在平片隐匿、重叠部位的轻微骨皮质中断也能为多层螺旋CT扫描所发现[2]; 老年人由于骨质疏松, 骨皮质菲薄, 局部的骨折线不明显, 前肋大部分由骨松质组成, 骨皮质菲薄, 且含有机质较多, 受力变形后常常观察不到骨折线, 或者仅表现为骨皮质的局部扭曲, 由于部分肋骨骨折没有明显的骨皮质中断, 在早期不能作为肋骨骨折的诊断依据, 随着骨折愈合过程中骨痂的形成和塑形, 才能在CT影像上被辨别, 从而诊断为肋骨骨折。因此胸部外伤早期影像学检查的结果不能作为法医临床鉴定的结论性依据[3]。
在临床治疗中, 主要是针对肋骨骨折的并发症进行治疗, 对肋骨骨折的数量关注度不够, 当发现与临床症状、体征相符合部位的明显骨折后, 对其它细微的骨折没有发现; 对不能立即确定为骨折的部位以骨皮质扭曲(变形、凹陷)报告或报告为可疑骨折建议复查。临床常规胸部CT扫描及骨重建采取5mm层厚, 当骨折线的走行方向与CT轴位近似平行时或由于CT的局部容积效应容易遗漏细微骨折, 而层厚大于1mm以上的CPR、MPR重建图像极易出现漏诊[4]。
在肋骨骨折或者疑似肋骨骨折的鉴定中, 需询问被鉴定人受伤过程, 详细询问胸部疼痛的部位、性质、与呼吸的关系及缓解方式等症状, 仔细检查胸部的体表损伤、压痛的部位、胸廓挤压征等体征。提高读片能力, 不仅要掌握肋骨骨折的各种表现形态, 还要注意肋骨周围软组织肿胀、胸膜下小血肿等间接征象。在审阅影像学资料时, 由于一张胶片往往有30帧以上甚至达64帧图像, 许多医院提供的是纸片而不是胶片, 图像分辨率远不及临床医生读片时所见, 所以当审阅的结果与影像学有出入时应当要求办案单位拷贝相应的CT数码图片送检或去医院调阅数码图片。需要特别注意的是, 在法医临床鉴定中, 虽然各种螺旋CT后处理技术的应用对及时发现和诊断肋骨骨折有及其重要的意义, 但是由于呼吸运动和扫描参数的不同对重建的图像有较大的影响, 有可能出现伪影和遗漏[5], 确诊肋骨骨折应当以轴位图像为准, 重建图像为辅。在初次受理鉴定时, 对被鉴定人应当要求在外伤后4w复查一次胸部CT, 并在告知单上注明复查时请医院采用薄层扫描, 有条件的被鉴定人可以在外伤后2、4w复查两次以动态观察, 当肋骨骨折数量有变化时更有利于说理分析。
在法医临床鉴定工作中, 特别是基层公安机关人体损伤程度鉴定中, 由于办案期限的限制, 委托单位往往希望在尽量短的时间内作出鉴定。过早地依据影像学检查结果出具鉴定意见容易因为肋骨骨折部位的漏诊导致鉴定意见出现错误。在外伤4w后复查CT再进行人体损伤程度鉴定, 能够依据骨痂的生长明确判断肋骨骨折的部位, 可以有效避免认定的损伤出现遗漏或鉴定意见出现错误。
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|